With the help of advanced technology in materials such as polymers and metals, new 3D reverse engineering software from Geomagic, and more-traditional CAD/CAM software, Cleveland Clinic researchers, led by staff member Dr. William A. Smith, are working toward the breakthrough that has been eluding the medical world for decades.
It has been more than 20 years since surgeons placed the country's first artificial heart in 61-year-old Barney Clark. The Washington dentist lived just 112 days after doctors implanted the Jarvik-7 device.
Although Clark's ordeal is not a fond memory for scientists and physicians searching for a way to cure patients with heart failure, technology has come a long way since then. There are now electrically powered devices, called Left Ventricular Assist Devices (LVAD) that can keep patients alive until a donor is found. But not every heart patient is an LVAD candidate. And there are at least 30,000 more people waiting for a transplant each year than there are hearts from donors.
These statistics have inspired medical institutions such as the Cleveland Clinic Foundation, an LVAD pioneer, to create a Total Artificial Heart (TAH) that will bring life to patients without access to a donor.
With the help of advanced technology in materials such as polymers and metals, new 3D reverse engineering software from Geomagic, and more-traditional CAD/CAM software, Cleveland Clinic researchers, led by staff member Dr. William A. Smith, are working toward the breakthrough that has been eluding the medical world for decades.
A Heart-Filled History and Future
Since it opened in 1921, the Cleveland Clinic has been an aggressive contributor to research and development for heart-failure patients. Cleveland Clinic surgeons have been performing transplants since 1984, and implanting LVADs since 1991. They began implanting a more advanced LVAD in 1997.
But the organization’s most ambitious project is the MagScrew Total Artificial Heart, being developed in collaboration with Foster-Miller Inc., which could eventually be implanted permanently.
"Unlike LVADs, which are designed to aid one ventricle of the native heart, our TAH is a device that replaces the sick natural ventricles and native valves of a patient," says Stephan Weber, senior research engineer in the Department of Biomedical Engineering at the Cleveland Clinic Foundation. "Applications for this system would exist for patients with end-stage heart failure who would not survive until a suitable heart donor is located for transplant or for patients who are not eligible for heart transplantation."
When implanted, the inlets to the artificial heart are connected to the natural atria; the outlets connect to the aorta (left) and pulmonary artery (right). Eventually, the Clinic’s TAH is fully implanted with no wires passing through the skin for a power source. Implanted with the heart are the controller, internal battery, compliance chamber and an energy transfer system.
Going with the Flow
One of the most critical issues with the TAH is how the blood flows through the device.
"Certain flow patterns have been proven to cause blood damage,” says Weber. “Features have been added to our model to improve the flow pattern through our pump."
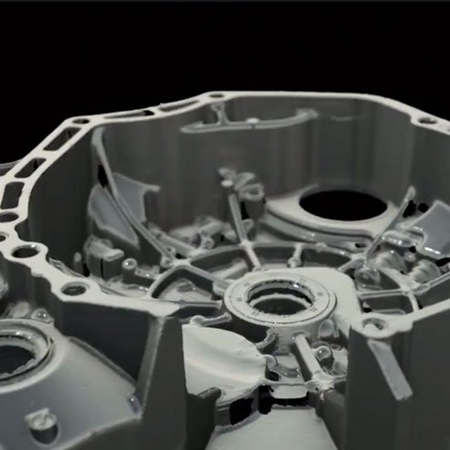
Cleveland Clinic researchers determined that the best way to ensure proper flow pattern was to reverse-engineer the complex geometries of the blood pump housings in the TAH. "We needed this model to be as accurate as possible to ensure proper blood flow within the chamber," Weber says.
Weber turned to Advanced Design Concepts (ADC), a 3D modeling and CAD service bureau in Pewaukee, Wis., to supply a surface model and a 3D solid model representation of the chamber.
Ergonomical Precision
Researchers sent ADC a plastic model of the internal volume of one of the blood pump chambers to make the computer models. The unusual shape makes it difficult to scan and generate an accurate 3D model for the device.
"The housing does not have a very mechanical shape," says Mark Schaefer, ADC president. "It flows more ergonomically than mechanically. A key feature in the housing design is the smooth transition from the inflow port to the main chamber and from the main chamber to the outlet port. This is what creates a smooth flow pattern for the blood. Modeling this as accurately as possible avoids dead zones of flow and blood clot formation."
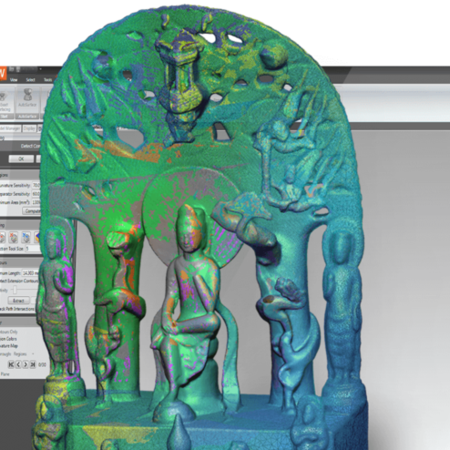
ADC began by painting the housing white and scanning it with an Atos white-light scanner. Engineers then used Geomagic Wrap software to convert the resulting scanned data into a 3D solid model.
Geomagic Wrap combines precise dimensional geometry and photometric color information in one process. The result is a true-to-life, accurate 3D model that can be imported into CAD software, used to drive a manufacturing device, or placed on the Internet for collaborative engineering and e-commerce applications. This automated process is what Geomagic calls 3D reverse engineering.
Ensuring Quality and Saving Time
For this application, ADC imported the Geomagic Wrap model into Pro/ENGINEER, the MCAD software used by the Cleveland Clinic. Once the Pro/ENGINEER model was completed, it was imported as an IGES file into Geomagic Control, software that allows automatic graphical comparisons between a CAD master model and the built part or object.
At the click of a mouse, Geomagic Control automatically aligned the CAD model with scanned point cloud data from the plastic TAH model. After ADC specified the level of tolerance, Qualify displayed a detailed color map showing different deviation levels. The software can also produce a green and red display that acts as a "go/no-go" gauge. Results can be documented automatically in web-ready HTML reports with annotated notes.
"In Control we were able to see errors in the Pro/ENGINEER model relative to the original plastic model," Schaefer says. "We corrected those and were able to get the model to within 0.010 of an inch of the original, which is what the Cleveland Clinic team had requested. The whole process took less than one day as opposed to what might have been weeks using the Pro/ENGINEER software alone."
A Large Hurdle Cleared
The end result for the Cleveland Clinic team was a 3D digital model almost identical to the original device.
"Geomagic’s precision helped us over one of the largest hurdles between the existing device and a TAH that can be manufactured accurately," says Weber. "The process ADC used saved both time and money. We had attempted to measure the geometry of the volume using a CMM machine, but this took too much time and the resulting model was not even close to being accurate enough."
With Geomagic Control, it was a quick and easy process to ensure that the 3D model was accurate. "The ability to switch back and forth between Pro/E and Geomagic Control with little hesitation in processing time saved literally days," says Schaefer.
Weber thinks that the 3D reverse engineering approach used by ADC brings the Cleveland Clinic a little closer to making its total artificial heart a reality. For heart patients, it could eventually mean the difference between life and death.